

Healing the Heart: Psychological and Respiratory Therapy for the 9/11 Rescue Workers
by Michael Magloire, ex WTC rescue worker and respiratory therapist


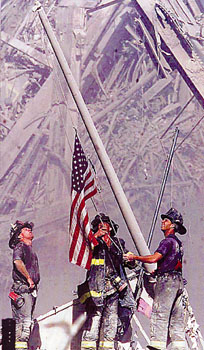
The terrorist attacks of September 11 were the most televised event in human history. Most people are still haunted by the sights and sounds of crashing planes, collapsing towers and terrified victims. I want to talk about memories that are not just visual, mediated terror amplified by the media, but olfactory, respiratory, deeply psychological memories embedded in the hearts and lungs of the rescue workers. You can walk away from your television set, but the rescue workers cannot walk away from their damaged lungs and broken hearts. Due to the force and magnitude of the impact, along with hundreds of gallons of jet fuel, New Yorkšs beloved landmark collapsed in utter chaos and destruction. Thousands of innocent people lost their lives. Unfortunately, the real damage occurred in the aftermath. Hundreds of rescue workers rushed to the scene as soon as the first plane flew into tower I: policeman, firefighters, Port Authority police, ambulance personnel, hospital staff and volunteers from all over the city. Not only did they have to deal with the death and destruction that surrounded them, but they also had to deal with the loss of friends and co-workers. Not surprisingly, this took a mental and physical toll on many of them. Some of them felt it right away, but a large amount of others experienced the effects months after September 11th. As national heroes, it is sometimes hard for these strong, brave men to admit their weaknesses, their fear, their nightmares. This paper will discuss the effects that this tragic day had on rescue workers, mentally and physically, and what could be done to improve their situation as well as prevent future problems.
My personal experience with the World Trade Center went as far back as 1994 when we were bombed for the first time by terrorists. I was employed at the time by the city as an Emergency Medical Technician and WTC, South Street Seaport was my stationed area from Monday through Friday 8am-430pm. I loved the area dearly. The job on the other hand wasn't that great, but it paid the bills. The majority of our calls consisted of minor fender benders, heat exhaustion and maybe a couple of baby deliveries, but nothing ever traumatic, until one morning when everything changed. It was 35 degrees, snowy and windy.
BBBBBBBOOOOOOOOOOMMMMMM was all my partner and I heard on that freezing day in February. When we saw an enormous cloud of smoke in the direction of the WTC, we grabbed our tech bags and went running to help. No time to drive the ambulance through because the streets were as chaotic as the LA riots of 1990. When we arrived at the tragic sight, we learned that there had been an explosion directly targeted to bring down the towers as an act of terrorism. I said to my partner, whošs name was asked to be left out: that we must transport as many people to the hospital as possible because I donšt think its over. I had a funny feeling the bombing wasnšt over. Hours went by and after hundreds of trips to the hospital, administration of oxygen, bandages, tourniquets, it was all over. When I got on the train to go home that night it was a relief. I stormed in my house to let my parents know that their son was o.k. I hadnšt any friends or family lost by this particular event, but I was too frightened to return to my post the following day. My supervisor understood and basically told me to take some time off. I took his advice and changed posts completely to a suburb in Queens where I enrolled in a Respiratory Therapist Program. I was touched by the miracles the therapists and the impact they had on the survivors, so I thought I should go for it. Not to mention how much safer their job was in the hospital as opposed to my station as a sitting duck by the WTC awaiting for my call. Over the years I have kept in touch with a number of friends who are still rescue workers, and here was their experience with 9/11.
CASE STUDIES:
1. Terence McArthur, a 10 year veteran for F.D.N.Y ladder 126 in Astoria Queens, was in bed at his North Babylon, home in Long Island when the terrorist attacks occurred. At approximately 9:01 am he received a call from a co-worker informing him of the first tower being hit by an airplane. His first instincts were to throw on his F.D.N.Y jacket, jump in the car and head for downtown in his suburban suv equipped with sirens and lights on the roof. By the time his commute was complete the second tower had already been hit. He fled in and began to help civilians in need and tried to evacuate as quick as possible. Less than 1 hour and down went the towers. Lucky for him he was carrying a woman from the 32nd floor to a rest stop at the time three blocks away. Devastation, anger, sadness and disgust were the feelings Terence was going through. He stated "I felt my heart stop." When all the smoke cleared, over 300 firefighters missing and presumed dead, 41 close friends of his and 13 close co-workers at the Astoria ladder 126.
As time went on, Terence felt as if it was his duty to help in the recovery efforts to find his buddies and fellow comrades. Terence worked at ground zero 7days a week 12-16 hours a day until November 28th when Mayor Giuliani assigned union workers to finish the recovery efforts, and wanted all the civil workers to get back to their regular work stations. "That fucking bastard, how can he take me from my friends" was Terence's way of expressing his anger towards Giuliani for making that decision. When that occurred Terence said he would dedicate his life to his fallen heroic friends by working overtime at the station house, followed by volunteering at his neighborhood firehouse in Long Island. Mrs. McArthur was sympathetic up until the Thanksgiving holiday. Their relationship began to crumble in little pieces. Terence would have constant nightmares the few nights he was home, and began to neglect his wife and 2 kids. "I would and still have nightmares of me and my friends drinking and playing poker on our off day at the volunteer firehouse," said Terence. He was very emotional during our interview which actually took place at the volunteer firehouse in Long Island. His wife is a stay at home mom and felt so neglected because of the lack of sex, companionship along with the emotional rollercoaster that she recently decided to file for divorce. When I asked Terence how he felt about that decision he said "fuck her, she will never understand the bond firefighters have for each other and I don’t want to be bothered." He began to get teary eyed and said sometimes he wishes he was up there with them. Terence is under bronchodilator therapy and is required to get a pulmonary function test later this month. He constantly complains of shortness of breath, chest tightness, and appears to be gray, flushed and dusky which is a sign of Chronic Bronchitis. These symptoms are directly related to post 9/11 with the exception of hypoxemia which is associated with low level carboxyhemaglobin in firefighters because of the nature of their profession. Before I concluded my interview I said a prayer for him and his family and Terence promised me that he will take advantage of the post psychological stress class offered by the city which was formed by the NYPD.
2. David Juste, a 5 year veteran of the N.Y.P.D, was actually stationed at the New York Downtown Hospital, in the area of the WTC. He, being a very lucky man that day, was helping others evacuate the building at the time the first tower was hit. The exact moment the second tower was hit he was in a state of shock. "I immediately grabbed two women who fell and we ran south toward Battery Park, boy was I scared shitless." David, who was trained in BLS certification and first aid, stayed near the park to help the needy victims. As soon as he decided to proceed on to the towers, they sadly came tumbling down. Shock, fear, tears couldn’t describe the way he felt at that moment. David also lost a total of 29 close friends ranging from firefighters, fellow police officers and hospital workers. David admitted to having sleepless nights because of nightmares stemming from the attack. He took advantage of the city funded counseling early in September and requested a temporary transfer to Brooklyn. His transfer was granted and David admitted to racially profiling Jews, Arabs, or any one with an Indian complexion, issuing summonses for no reason, and constantly threatening to arrest if they talked back. "It was the worst time of my life; here I am an African American who is so against racism, especially being a victim of it at times myself, and I’m wrongfully using my badge to attack those who look like Osama Bin Laden."
"My partner eventually took the wheel when we worked together and said he would report me if I didn’t transfer back to the WTC" were the words that came out of David’s mouth when he, like Terence, began to cry like a newborn baby. David, an asthmatic since birth, said he thought he had his asthma under control until the terrorist attacks. He said he had to improve to a more potent bronchodilator opposed to the one he has been using for 15 years. He has a new Pulmonologist and is going through many appropriate diagnostic measures and treatments for his asthma. Eventually David did transfer back to the hospital post and is seeking more psychological help offered by the city. He also stated to me that the 9/11 attacks still have him "bugging" and he is considering moving down south.
3. Jason Little, a Paramedic for 9 years with the New York City Emergency Services, is a very close friend of mine. He is stationed near the WTC, but Jason missed most of the "excitement" that day. At exactly 9 am, as one of the first emergency workers on the scene, he took three of the most critical patients to a nearby hospital, and by the time he had returned to the WTC, both towers had vanished. He quickly assisted in the triage for the employees and fellow rescue workers, the few that did make it. Jason is very healthy and doesn’t experience any respiratory difficulties at this time but did admit to frequent nightmares, in which he cared not to go into details. However what did and does annoy Jason the most is the respect that the country has denied him and all EMS workers. He stated "I was working hard and doing my best just as NYPD, FDNY workers did and our department lost 16 paramedics and technicians but you don’t see our names on any t-shirts!" He got so emotional and stated that the news doesn’t recognize them at all. I tried to console him but he raced out of the room and said this would be his last year in the department.
4. Rhonda Lewis, a stranger to me, but everyone’s neighbor around ground zero, was spotted feeding the pigeons in the park near City Hall and was kind enough to let me interview her. I wanted to interview a resident to see if they suffered the same respiratory problems as the rescue workers. Mrs. Lewis is a COPD’er with emphysema and her doctor stated it would be better if she relocated for medical reasons. She was outraged and disgusted with his request and changed doctors because of the love she has for the area. Mrs. Lewis stated "I’m saddened by the attacks of 9/11 and the change in the world we live in. I have never seen this city turn into a ghost town. Nearly10 months after the attacks and we still are breathing in nasty debris, it makes me cry at times especially since my last family member died 3 days before the attack and I’m now officially alone in Gotham City, awaiting gods calling. My advice to you son is to live a full and righteous life, I feel so bad for the young ones like yourself that we lost." Since she was a total stranger. she really touched my heart and I bought her coffee and went on my way.
From these interviews it appears that most of the rescue workers are suffering from PTSD as well as respiratory problems. Let me clarify the symptoms.
The diagnosis:
.
occurring when a person has been exposed to a traumatic event in which he or
she experienced, witnessed or was confronted with an event or events that
involved actual death or serious injury or a threat to the physical integrity of
self. In addition, the person’s response involved intense fear, helplessness and
horror.
The diagnosis:

The following is a detailed description of the symptoms, progression and treatment modalities of these diseases:
Post-Traumatic Stress Disorder: PTSD, is a psychiatric disorder that can occur following the experience or witnessing of life-threatening events such as military combat, natural disasters, terrorist incidents, serious accidents, or violent personal assaults like rape. People who suffer from PTSD often relive the experience through nightmares and flashbacks, have difficulty sleeping, and feel detached or estranged, and these symptoms can be severe enough and last long enough to significantly impair the personšs daily life. PTSD is marked by clear biological changes as well as psychological symptoms. PTSD is complicated by the fact that it frequently occurs in conjunction with related disorders such as depression, substance abuse, problems of memory and cognition, and other problems of physical and mental health. The disorder is also associated with impairment of the personšs ability to function in social or family life, including occupational instability, marital problems and divorces, family discord, and difficulties in parenting.
PTSD is not a new disorder. There are written accounts of similar symptoms that go back to ancient times, and there is clear documentation in the historical medical literature starting with the Civil War, where a PTSD-like disorder was known as "Da Costašs Syndrome."There are particularly good descriptions of post-traumatic stress symptoms in the medical literature on combat veterans of World War II and on Holocaust survivors. Careful research and documentation of PTSD began in earnest after the Vietnam War. The National Vietnam Veterans Study estimated in 1988 that the prevalence of PTSD in that group was 15.2% at that time, and that 30% had experienced the disorder at some point since returning from Vietnam. PTSD has subsequently been observed in all veterans populations that have been studied, including World War II, Korean conflict, and Persian Gulf, and in United Nations peacekeeping forces deployed to other war zones around the world. Although there are unique cultural- and gender-based aspects to the disorder, it occurs in both men and women, adults and children, Western and non-Western cultural groups, and all socioeconomic strata. A national study of Americans conducted in 1995 estimated that the lifetime prevalence of PTSD was 5% in men and 10% in women. Most people who are exposed to a traumatic, stressful event experience some of the symptoms of PTSD in the days and weeks following exposure. Available data suggest that about 8% of men and 20% of women go on to develop PTSD, and roughly 30% of these individuals develop a chronic form that persists throughout their lifetimes.
The course of chronic PTSD usually involves periods of symptom increase followed by remission or decrease, although for some individuals symptoms may be unremitting and severe. Some older patients who report a lifetime of only mild symptoms have experienced significant increases following retirement, severe medical illness in themselves or their spouses, or reminders of the trauma such as reunions or media broadcasts of the anniversaries of the events. In recent years a great deal of research has been aimed at development and testing of reliable assessment tools. It is generally thought that the best way to diagnose PTSD or any psychiatric disorder, for that matter is to combine findings from structured interviews and questionnaires with physiological assessments. A multi-method approach is especially helpful to address concerns that some patients might be either denying or exaggerating their symptoms. An estimated 7.8 percent of Americans will experience PTSD at some point in their lives, with women (10.4%) twice as likely as men (5%) to have PTSD. About 3.6 percent of U.S. adults ages 18 to 54 (5.2 million people) have PTSD during the course of a given year. This represents a small proportion of those who have experienced a traumatic event at some point in their lives, for 60.7% of men and 51.2% of women reported at least one traumatic event.
The traumatic events most often associated with PTSD are: for men: rape, combat exposure, childhood neglect, and childhood physical abuse. For women :rape, sexual molestation, physical attack, being threatened with a weapon, and childhood physical abuse. About 30 percent of the men and women who have spent time in war zones experience PTSD. An additional 20 to 25 percent have had partial PTSD at some point in their lives. Thus more than half of all male Vietnam veterans and almost half of all female Vietnam veterans have experienced "clinically serious stress reaction symptoms." PTSD has also been detected among veterans of the Gulf War, with some estimates running as high as 8 percent. People who are more likely than others to experience PTSD are those who experience greater stressor magnitude and intensity, unpredictability, uncontrollability , sexual (as opposed to nonsexual) victimization, real or perceived responsibility, and betrayal; those with prior vulnerability factors such as genetics, early age of onset and longer-lasting childhood trauma, lack of functional social support, and concurrent stressful life events; those who report greater perceived threat or danger, suffering or being upset, terror, and horror or fear; those with a social environment which produces shame, guilt, stigmatization, or self-hatred. PTSD is associated with a number of distinctive neurobiological and physiological changes.
PTSD may be associated with stable neurobiological alterations in both the central and autonomic nervous systems, such as altered brainwave activity, decreased volume of the hippocampus, and abnormal activation of the amygdala. Both of these brain structures are involved in the processing and integration of memory . The amygdala has also been found to be involved in coordinating the body's fear response. Psycho physiological alterations associated with PTSD include hyper arousal of the sympathetic nervous system, increased sensitivity of the startle reflex, and sleep abnormalities. People with PTSD tend to have abnormal levels of key hormones involved in response to stress. Thyroid function seems to be enhanced in people with PTSD. Some studies have shown that cortical levels are lower than normal and epinephrine and nor epinephrine are higher than normal. People with PTSD also continue to produce higher than normal levels of natural opiates after the trauma has passed. An important finding is that the neurohormonal changes seen in PTSD are distinct from, and actually opposite to, those seen in major depression; also, the distinctive profile associated with PTSD is seen in individuals who have both PTSD and depression. PTSD is associated with increased likelihood of co-occurring psychiatric disorders. In a large-scale study, 88 percent of men and 79 percent of women with PTSD met criteria for another psychiatric disorder. The co-occurring disorders most prevalent for men with PTSD were alcohol abuse or dependence (51.9 percent), major depressive episode (47.9 percent), conduct disorder (43.3 percent), and drug abuse and dependence (34.5 percent). The disorders most frequently co-morbid with PTSD among women were major depressive disorder (48.5 percent), simple phobia (29 percent), social phobia (28.4 percent) and alcohol abuse/dependence (27.9 percent).
PTSD also makes a significant impact on psychosocial functioning, independent of co-morbid conditions. For instance, Vietnam veterans with PTSD were found to have profound and pervasive problems in their daily lives. These included problems in family and other interpersonal relationships, employment, and involvement with the criminal justice system. Headaches, gastrointestinal complaints, immune system problems, dizziness, chest pain, or discomfort in other parts of the body are common in people with PTSD. Often, medical doctors treat the symptoms without being aware that they stem from PTSD. Most people who are exposed to a traumatic stressor experience some of the symptoms of PTSD in the days and weeks following exposure. Available data suggest that among individuals who go on to develop PTSD, roughly 30 percent develop a chronic form that persists throughout an individualšs lifetime. The course of chronic PTSD usually has periods of symptom exacerbation and remission or decrease, although for some individuals symptoms may persist at an unremitting, severe level. Some older patients who report a lifetime of no or only mild symptoms have experienced exacerbations of symptoms following retirement, severe medical illness in themselves or their spouses, or exposure to reminders of the trauma (such as reunions or media broadcasts of the anniversaries of the event ).
PTSD is treated by a variety of forms of psychotherapy and drug therapy. There is no definitive treatment, and no cure, but some treatments appear to be quite promising, especially cognitive-behavioral therapy, group therapy, and exposure therapy, in which the patient repeatedly relives the frightening experience under controlled conditions to help him or her work throughout the trauma. Studies have also shown that medications help ease associated symptoms of depression and anxiety and help ease sleep. The most widely-used drug treatments for PTSD are the selective serotonin reuptake inhibitors, such as Prozac and Zoloft. At present, cognitive-behavioral therapy appears to be somewhat more effective than drug therapy, but it would be premature to conclude that drug therapy is less effective overall since drug trials for PTSD are at a very early stage. Drug therapy definitely appears to be highly effective for some individuals and is helpful for many more. Also, the recent findings on the biological changes associated with PTSD have spurred new research into drugs that target these biological changes, which may lead to much increased efficacy.
The following is a breakdown of the respiratory problems most common to the 9/11 rescue workers:
Chronic Obstructive Pulmonary Disease: COPD will play an enormous role on our post 9/11 rescue workers and people who generally work or live in the downtown area of ground zero.
Asthma: Being the most simplest of them all is a heterogeneous disorder characterized by cough, wheeze, dyspnea, and variable degrees of reversible airflow obstruction. Acute intermittent asthma is easy to define and diagnose. Attacks are characterized by the sudden onset of dyspnea, cough and wheeze, followed by complete or nearly complete cessation of symptoms and a return to normal airflow. Reversible airflow obstruction which usually follows the use of bronchodilators may sometimes subside spontaneously, as in extrinsic induced asthma. Extrinsic induced asthma has a great deal to do with the environment that we live in. The amount of (sooche) which is a thick substance in the air post the tragic events of the remnants of WTC is a great candidate to cause extrinsic asthma.
Emphysema: Characterized clinically by progressive dyspnea and variable cough. Physiologically, emphysema is characterized by hyperinflation followed by chronic progressive airflow obstruction. In fact, an increased total lung capacity, associated with reduced elastic recoil in the lung area is found in the earliest stages of emphysema.
Chronic bronchitis: So-called chronic bronchitis is very similar to asthma. Shortness of breath, wheeze, coughing and sputum production for many months over a course of 9 months to a year. Many of the connections with post 9/11 are consolidation in the inferior lobes of the lungs which decrease efficient values of pulmonary function testing.
According to the diseases described above, airflow obstruction is a common disorder within our rescue workers today as a result of post 9/11.
To help solve all the post traumatic and respiratory problems I have just described, I have designed my own utopian 9/11 Rehabilitation Center. We would set up a significant program here for those affected and those in the NYPD,EMS,FDNY who will possibly have to encounter casualties as severe as this one was in the near future.
 With continued threats
of terrorism, including more devastating attacks using weapons of mass
destruction, it is imperative we give our rescue workers the treatment
and support they need before, during and after catastrophes. They are
our first, and often last line of defense.
With continued threats
of terrorism, including more devastating attacks using weapons of mass
destruction, it is imperative we give our rescue workers the treatment
and support they need before, during and after catastrophes. They are
our first, and often last line of defense.Bibliography
1-Burton, George, G (1991) Respiratory Care a guide to clinical practice, Penn, J.B. Lippincott Company.
2- Editors of NY (2001) September 11, 2001: A Record of Tragedy, Heroism and Hope. NY: Harry N. Abrams, Inc.
3- Franco, M. (2001) a collection of newspaper front pages. Kansas City: Andrews Mcneil Publshing.
4-Malley, William, J (1990) Clinical Blood Gases, Penn, W.B. Saunders Company.
5-McPherson, Steven, P (1990) Respiratory Therapy Equipment, St Louis, The C.V. Mosby Company.
6-Picciotto, Richard (2002) Last Man Down. NY: Burkley Books.
7-Pilbeam, Susan, P(1992) Mechanical Ventilation, Chicago, Mosby Year Book
8- Talbot, S., Chanda, N. (2002) The Age of Terror. New Haven: Basic Books.
9-Whitaker, Kent (1992) Comprehensive perinatal and pediatric respiratory care, Utah, Delmar Publishers INC.
Internet Sources:
Understanding PTSD. Retrieved July 20, 2002 from http://www.zoloft.com/index.asp?
Post Traumatic Stress Disorder. Retrieved July 20, 2002 from http://www.nami.org/helpline/ptsd.html
Post Traumatic Stress Disorder. Retrieved July 20, 2002 from http://www.ncptsd.org/treatment/literature/overview
PTSD. Retrieved July 20, 2002 from http://www.ptsdalliance.org/home2.html
What Is Post Traumatic Stress Disorder. Retrieved July 20, 2002 from http://okok.essortment.com/whatispaottr_rfxg.htm
Post Traumatic Stress Disorder. Retrieved July 20, 2002 from http://www.nlm.nih.gov/medlineplus/posttraumaticstressdisorder.html
Interviews: Names altered to protect privacy
1. Interview with Terrence McArthur (Firefighter) by Michael Magloire, (6/09/02)
2. Interview with Jason Littles (EMS Paramedic) by Michael Magloire, (6/14/02)
3. Interview with David Juste (Policeman) by Michael Magloire, (6/23/02)
4. Interview with Rhonda Lewis (Manhattan Resident) by Michael Magloire, (6/23/02)
5. Interview with Mr. Magloire (Ex EMS worker) by Michael Magloire, (7/23/0